Abstract
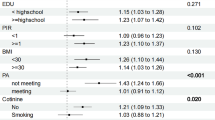
The usage of glyphosate is increasing worldwide. Glyphosate and its major metabolite, aminomethylphosphonic acid (AMPA), are of potential toxicological concern in unknown chronic kidney disease (CKDu). As with Cd and other elements, glyphosate exposure has been reported as risk factor for CKDu in farmers. This study aimed to evaluate the influence of co-exposure to glyphosate and metals or metalloids in chronic kidney disease (CKD). In this study, the urine samples from 55 patients with CKD and 100 participants without CKD were analyzed for glyphosate, arsenic (As), cadmium (Cd), and lead (Pb) concentrations, and estimated glomerular filtration rate (eGFR). Negative associations between glyphosate, AMPA, As, and Cd concentrations in the urine and eGFR were found for study subjects (p < 0.05). With regard to the effect of co-exposure, the odds ratios (OR) for subjects with an eGFR of < 60 mL/min/1.73 m2 was significant because of the high Cd concentration (> 1 μg/g creatinine; OR = 7.57, 95% CI = 1.91–29.95). With regard to the effect of co-exposure, the OR for subjects with an of eGFR < 45 mL/min/1.73 m2 was significant at high glyphosate concentration (> 1 μg/g creatinine; OR = 1.57, 95% CI = 1.13–2.16) and As concentration (> 1 μg/g creatinine; OR = 1.01, 95% CI = 1.00–1.02). These results showed that glyphosate, AMPA, As, and Cd have an effect on CKD; notably, Cd, As, and glyphosate exposure can be important risk factors after stage 3a of CKD, and that there was a co-exposure effect of As and glyphosate in CKD after stage 3b. The potential health impacts of glyphosate should be considered, especial for patients with CKD and eGFR below 45 mL/min/1.73 m2.

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Abdul KSM, De Silva P, Ekanayake E, Thakshila W, Gunarathna SD, Gunasekara T et al (2021) Occupational paraquat and glyphosate exposure may decline renal functions among rural farming communities in Sri Lanka. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph18063278
Aguilera I, Daponte A, Gil F, Hernández AF, Godoy P, Pla A et al (2008) Biomonitoring of urinary metals in a population living in the vicinity of industrial sources: a comparison with the general population of Andalusia. Spain Sci Total Environ 407(1):669–678
Anadon A, Martinez-Larranaga M, Martinez M, Castellano V, Martínez M, Martin M et al (2009) Toxicokinetics of glyphosate and its metabolite aminomethyl phosphonic acid in rats. Toxicology Lett 190(1):91–95
Babich R, Ulrich JC, Ekanayake E, Massarsky A, De Silva P, Manage PM et al (2020) Kidney developmental effects of metal-herbicide mixtures: implications for chronic kidney disease of unknown etiology. Environ Int. https://doi.org/10.1016/j.envint.2020.106019
Baeyens W, Vrijens J, Gao Y, Croes K, Schoeters G, Den Hond E et al (2014) Trace metals in blood and urine of newborn/mother pairs, adolescents and adults of the Flemish population (2007–2011). Int J Hyg Environ Health 217(8):878–890
Bai SH, Ogbourne SM (2016) Glyphosate: environmental contamination, toxicity and potential risks to human health via food contamination. Environ Sci Pollut Res Int 23(19):18988–19001. https://doi.org/10.1007/s11356-016-7425-3
Batista BL, Rodrigues JL, Nunes JA, de Oliveira Souza VC, Barbosa F (2009) Exploiting dynamic reaction cell inductively coupled plasma mass spectrometry (DRC-ICP-MS) for sequential determination of trace elements in blood using a dilute-and-shoot procedure. Anal Chim Acta 639(1):13–18. https://doi.org/10.1016/j.aca.2009.03.016
Cai R, Zheng YF, Bu JG, Zhang YY, Fu SL, Wang XG et al (2017) Effects of blood lead and cadmium levels on homocysteine level in plasma. Eur Rev Med Pharmacol Sci 21(1):162–166
Chang K, Wu IW, Huang BR, Juang JG, Wu JC, Chang SW et al (2018) Associations between water quality measures and chronic kidney disease prevalence in Taiwan. Int J Environ Res Public Health 15(12):2726
Chang ET, Delzell E (2016) Systematic review and meta-analysis of glyphosate exposure and risk of lymphohematopoietic cancers. J Environ Sci Health - B Pestic Food Contam Agric Wastes 51(6):402–434. https://doi.org/10.1080/03601234.2016.1142748
Chang FC, Simcik MF, Capel PD (2011) Occurrence and fate of the herbicide glyphosate and its degradate aminomethylphosphonic acid in the atmosphere. Environ Toxicol Chem 30(3):548–555. https://doi.org/10.1002/etc.431
Cheng YY, Chang YT, Cheng HL, Shen KH, Sung JM, Guo HR (2018) Associations between arsenic in drinking water and occurrence of end-stage renal disease with modifications by comorbidities: a nationwide population-based study in Taiwan. Sci Total Environ 626:581–591. https://doi.org/10.1016/j.scitotenv.2018.01.043
Conrad A, Schröter-Kermani C, Hoppe HW, Rüther M, Pieper S, Kolossa-Gehring M (2017) Glyphosate in German adults–Time trend (2001 to 2015) of human exposure to a widely used herbicide. Int J Hyg Environ Health 220(1):8–16
Correa-Rotter R, Wesseling C, Johnson RJ (2014) CKD of unknown origin in Central America: the case for a Mesoamerican nephropathy. Am J Kidney Dis 63(3):506–520
Duke SO, Powles SB (2008) Glyphosate: a once-in-a-century herbicide. Pest Manag Sci 64(4):319–325. https://doi.org/10.1002/ps.1518
EFSA (2015). "Glyphosate: EFSA updates toxicological profile." from https://www.efsa.europa.eu/en/press/news/151112
EFSA (2018). "Pesticides in food." from https://www.food.gov.uk/business-guidance/pesticides-in-food.
Feng W, Cui X, Liu B, Liu C, Xiao Y, Lu W et al (2015) Association of urinary metal profiles with altered glucose levels and diabetes risk: a population-based study in China. PLoS ONE 10(4):e0123742
Gao H, Chen J, Ding F, Chou X, Zhang X, Wan Y et al (2019) Activation of the N-methyl-d-aspartate receptor is involved in glyphosate-induced renal proximal tubule cell apoptosis. J Appl Toxicol 39(8):1096–1107. https://doi.org/10.1002/jat.3795
George J, Prasad S, Mahmood Z, Shukla Y (2010) Studies on glyphosate-induced carcinogenicity in mouse skin: a proteomic approach. J Proteom 73(5):951–964. https://doi.org/10.1016/j.jprot.2009.12.008
González-Ortega E, Piñeyro-Nelson A, Gómez-Hernández E, Monterrubio-Vázquez E, Arleo M, Dávila-Velderrain J et al (2017) Pervasive presence of transgenes and glyphosate in maize-derived food in Mexico. J Agroecol Sust Food Syst 41(9–10):1146–1161
Gunatilake S, Seneff S, Orlando L (2019) Glyphosate’s synergistic toxicity in combination with other factors as a cause of chronic kidney disease of unknown origin. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph16152734
Heitland P, Köster HD (2006) Biomonitoring of 30 trace elements in urine of children and adults by ICP-MS. Clin Chim Acta 365(1–2):310–318
Helander M, Saloniemi I, Saikkonen K (2012) Glyphosate in northern ecosystems. Trends Plant Sci 17(10):569–574. https://doi.org/10.1016/j.tplants.2012.05.008
Herrera-Valdes R, Almaguer-Lopez MA, Orantes-Navarro CM, Lopez-Marin L, Brizuela-Diaz EG, Bayarre-Vea H et al (2019) Epidemic of chronic kidney disease of nontraditional etiology in el Salvador: integrated health sector action and south-south cooperation. MEDICC Rev 21(4):46–52
Honeycutt Z, Rowlands H (2014) Glyphosate testing report: findings in American mothers’ breast milk, urine and water. Moms Across America and Sustainable Pulse.
Hu J, Lesseur C, Miao Y, Manservisi F, Panzacchi S, Mandrioli D et al (2021) Low-dose exposure of glyphosate-based herbicides disrupt the urine metabolome and its interaction with gut microbiota. Sci Rep. https://doi.org/10.1038/s41598-021-82552-2
Indirakshi J, Sunnesh A, Aruna M, Reddy MH, Kumar AC, Chandra VS et al (2017) Toxic epidermal necrolysis and acute kidney injury due to glyphosate ingestion. Indian J Crit Care Med 21(3):167–169. https://doi.org/10.4103/ijccm.IJCCM_423_16
Jansons M, Pugajeva I, Bartkevics V (2018) Occurrence of glyphosate in beer from the Latvian market. Food Addit Contam Part A Chem Anal Control Expo Risk Assess 35(9):1767–1775. https://doi.org/10.1080/19440049.2018.1469051
Jayasumana C, Gunatilake S, Senanayake P (2014) Glyphosate, hard water and nephrotoxic metals: are they the culprits behind the epidemic of chronic kidney disease of unknown etiology in Sri Lanka? Int J Environ Res Public Health 11(2):2125–2147. https://doi.org/10.3390/ijerph110202125
Jayasumana C, Fonseka S, Fernando A, Jayalath K, Amarasinghe M, Siribaddana S et al (2015a) Phosphate fertilizer is a main source of arsenic in areas affected with chronic kidney disease of unknown etiology in Sri Lanka. Springerplus 24(4):90. https://doi.org/10.1186/s40064-015-0868-z
Jayasumana C, Gunatilake S, Siribaddana S (2015b) Simultaneous exposure to multiple heavy metals and glyphosate may contribute to Sri Lankan agricultural nephropathy. BMC Nephrol 16:103. https://doi.org/10.1186/s12882-015-0109-2
Jayasumana C, Paranagama P, Agampodi S, Wijewardane C, Gunatilake S, Siribaddana S (2015c) Drinking well water and occupational exposure to Herbicides is associated with chronic kidney disease, in Padavi-Sripura,Sri Lanka. Environ Health. https://doi.org/10.1186/1476-069X-14-6
Jha V, Garcia-Garcia G, Iseki K, Li Z, Naicker S, Plattner B et al (2013) Chronic kidney disease: global dimension and perspectives. The Lancet 382(9888):260–272. https://doi.org/10.1016/S0140-6736(13)60687-X
Kimura T, Yokoyama T, Tanemoto M (2020) Renal tubular injury by glyphosate-based herbicide. Clin Exp Nephrol. https://doi.org/10.1007/s10157-020-01962-0
Krüger M, Schledorn P, Schrödl W, Hoppe H-W, Lutz W, Shehata AA (2014) Detection of glyphosate residues in animals and humans. J Environ Anal Toxicol. https://doi.org/10.4172/2161-0525.1000210
Liao KW, Pan WH, Liou SH, Sun CW, Huang PC, Wang SL (2019) Levels and temporal variations of urinary lead, cadmium, cobalt, and copper exposure in the general population of Taiwan. Environ Sci Pollut Res 26(6):6048–6064. https://doi.org/10.1007/s11356-018-3911-0
Mills PJ, Kania-Korwel I, Fagan J, McEvoy LK, Laughlin GA, Barrett-Connor E (2017) Excretion of the Herbicide Glyphosate in Older Adults Between 1993 and 2016. JAMA 318(16):1610–1611. https://doi.org/10.1001/jama.2017.11726
Morton J, Tan E, Leese E, Cocker J (2014) Determination of 61 elements in urine samples collected from a non-occupationally exposed UK adult population. Toxicol Lett 231(2):179–193
Mueangkhiao P, Siviroj P, Sapbamrer R, Khacha-Ananda S, Lungkaphin A, Seesen M et al (2020) Biological variation in kidney injury and kidney function biomarkers among farmers in Lamphun province. Thailand. Environ Sci Pollut Res Int 27(11):12386–12394. https://doi.org/10.1007/s11356-020-07661-3
Myers JP, Antoniou MN, Blumberg B, Carroll L, Colborn T, Everett LG et al (2016) Concerns over use of glyphosate-based herbicides and risks associated with exposures: a consensus statement. J Environ Health 15(1):19
Niemann L, Sieke C, Pfeil R, Solecki R (2015) A critical review of glyphosate findings in human urine samples and comparison with the exposure of operators and consumers. J Für Verbraucherschutz Und Lebensmittelsicherheit 10(1):3–12. https://doi.org/10.1007/s00003-014-0927-3
Nishijo M, Suwazono Y, Ruangyuttikarn W, Nambunmee K, Swaddiwudhipong W, Nogawa K et al (2014) Risk assessment for Thai population: benchmark dose of urinary and blood cadmium levels for renal effects by hybrid approach of inhabitants living in polluted and non-polluted areas in Thailand. BMC Public Health 14(1):702
Palmer CD, Lewis ME, Geraghty CM, Barbosa F, Parsons PJ (2006) Determination of lead, cadmium and mercury in blood for assessment of environmental exposure: a comparison between inductively coupled plasma–mass spectrometry and atomic absorption spectrometry. Spectrochim Acta Part B at Spectrosc 61(8):980–990. https://doi.org/10.1016/j.sab.2006.09.001
Riede S, Toboldt A, Breves G, Metzner M, Köhler B, Bräunig J et al (2016) Investigations on the possible impact of a glyphosate-containing herbicide on ruminal metabolism and bacteria in vitro by means of the “Rumen Simulation Technique.” J Appl Microbiol. https://doi.org/10.1111/jam.13190
Rodrigues NR, de Souza APF (2018) Occurrence of glyphosate and AMPA residues in soy-based infant formula sold in Brazil. Food Addit Contam A 35(4):723–730
Rueda-Ruzafa L, Cruz F, Roman P, Cardona D (2019) Gut microbiota and neurological effects of glyphosate. Neurotoxicology. https://doi.org/10.1016/j.neuro.2019.08.006
Ruuskanen S, Rainio MJ, Gómez-Gallego C, Selenius O, Salminen S, Collado MC et al (2020) Glyphosate-based herbicides influence antioxidants, reproductive hormones and gut microbiome but not reproduction: a long-term experiment in an avian model. Environ Pollut. https://doi.org/10.1016/j.envpol.2020.115108
Ruwanpathirana T, Senanayake S, Gunawardana N, Munasinghe A, Ginige S, Gamage D et al (2019) Prevalence and risk factors for impaired kidney function in the district of Anuradhapura Sri Lanka: a cross-sectional population-representative survey in those at risk of chronic kidney disease of unknown aetiology. BMC Public Health. https://doi.org/10.1186/s12889-019-7117-2
Sabath E, Robles-Osorio ML (2012) Renal health and the environment: heavy metal nephrotoxicity. Nefrologia 32(3):279–286. https://doi.org/10.3265/Nefrologia.pre2012.Jan.10928
Samsel A, Seneff S (2013) Glyphosate, pathways to modern diseases II: Celiac sprue and gluten intolerance. Interdiscip Toxicol 6(4):159–184. https://doi.org/10.2478/intox-2013-0026
Schaeffer JW, Adgate JL, Reynolds SJ, Butler-Dawson J, Krisher L, Dally M et al (2020) A pilot study to assess inhalation exposures among sugarcane workers in guatemala: implications for chronic kidney disease of unknown origin. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17165708
Seneff S, Orlando L (2018) Is glyphosate a key factor in Mesoamerican nephropathy. J Environ Anal Toxicol. https://doi.org/10.4172/2161-0525.1000542
Silva V, Montanarella L, Jones A, Fernández-Ugalde O, Mol HGJ, Ritsema CJ et al (2018) Distribution of glyphosate and aminomethylphosphonic acid (AMPA) in agricultural topsoils of the European Union. Sci Total Environ 15(621):1352–1359. https://doi.org/10.1016/j.scitotenv.2017.10.093
Smpokou ET, Gonzalez-Quiroz M, Martins C, Alvito P, Le Blond J, Glaser J et al (2019) Environmental exposures in young adults with declining kidney function in a population at risk of Mesoamerican nephropathy. Occup Environ Med 76(12):920–926. https://doi.org/10.1136/oemed-2019-105772
Tellez-Plaza M, Navas-Acien A, Crainiceanu CM, Guallar E (2008) Cadmium exposure and hypertension in the 1999–2004 national health and nutrition examination survey (NHANES). Environ Health Perspect 116(1):51–56. https://doi.org/10.1289/ehp.10764
Tizhe EV, Ibrahim ND, Fatihu MY, Ambali SF, Igbokwe IO, Tizhe UD (2020) Effect of zinc supplementation on chronic hepatorenal toxicity following oral exposure to glyphosate-based herbicide (Bushfire(R)) in rats. J Int Med Res 48(5):1–15. https://doi.org/10.1177/0300060520925343
Trasande L, Aldana SI, Trachtman H, Kannan K, Morrison D, Christakis DA et al (2020) Glyphosate exposures and kidney injury biomarkers in infants and young children. Environ Pollut. https://doi.org/10.1016/j.envpol.2019.113334
Tsai CC, Wu CL, Kor CT, Lian IB, Chang CH, Chang TH et al (2018) Prospective associations between environmental heavy metal exposure and renal outcomes in adults with chronic kidney disease. Nephrol 23(9):830–836. https://doi.org/10.1111/nep.13089
Wang D, Zhang G, Zhang W, Luo J, Zhu L, Hu J (2019) Successful extracorporeal membrane oxygenation support for severe acute diquat and glyphosate poisoning: A case report. Medicine (baltimore). https://doi.org/10.1097/MD.0000000000014414
Wang R, Chen J, Ding F, Zhang L, Wu X, Wan Y et al (2021) Renal tubular injury induced by glyphosate combined with hard water: the role of cytosolic phospholipase A2. Ann Transl Med. https://doi.org/10.21037/atm-20-7739
Wilke RA, Qamar M, Lupu RA, Gu S, Zhao J (2019) Chronic kidney disease in agricultural communities. Am J Med. https://doi.org/10.1016/j.amjmed.2019.03.036
Wimalawansa S, Wimalawansa S (2014) Impact of changing agricultural practices on human health: chronic kidney disease of multi-factorial origin in Sri Lanka. Wudpecker J Agric Res 3(5):110–124
Wimalawansa SJ (2016) The role of ions, heavy metals, fluoride, and agrochemicals: critical evaluation of potential aetiological factors of chronic kidney disease of multifactorial origin (CKDmfo/CKDu) and recommendations for its eradication. Environ Geochem Health 38(3):639–678. https://doi.org/10.1007/s10653-015-9768-y
Wu CY, Wong CS, Chung CJ, Wu MY, Huang YL, Ao PL et al (2019) The association between plasma selenium and chronic kidney disease related to lead, cadmium and arsenic exposure in a Taiwanese population. J Hazard Mater. https://doi.org/10.1016/j.jhazmat.2019.04.082
Yang X, Wang F, Bento CPM, Xue S, Gai L, van Dam R et al (2015) Short-term transport of glyphosate with erosion in Chinese loess soil — A flume experiment. Sci Total Environ 512–513:406–414. https://doi.org/10.1016/j.scitotenv.2015.01.071
Zhang L, Ding F, Wang R, Wu X, Wan Y, Hu J et al (2021) Involvement of mitochondrial fission in renal tubular pyroptosis in mice exposed to high and environmental levels of glyphosate combined with hard water. Environ Pollut. https://doi.org/10.1016/j.envpol.2021.117082
Zoller O, Rhyn P, Rupp H, Zarn JA, Geiser C (2018) Glyphosate residues in Swiss market foods: monitoring and risk evaluation. Food Addit Contam Part B Surveil 11(2):83–91. https://doi.org/10.1080/19393210.2017.1419509
Zoller O, Rhyn P, Zarn JA, Dudler V (2020) Urine glyphosate level as a quantitative biomarker of oral exposure. Int J Hyg Environ Health. https://doi.org/10.1016/j.ijheh.2020.113526
Acknowledgements
We are in great debt to Division of Nephrology, Department of Internal Medicine, National Cheng Kung University Hospital for sampling assistance and our colleagues at the Research Center of Environmental Trace Toxic Substances, National Cheng Kung University Medical College for analytical assistance.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Junne-Ming Sung contributed to conceptualization, methodology, validation, subjects’ recruitment; Wei-Hsiang Chang, Chung Yu Chen contributed to formal analysis, writing; Kuan-Hung Liu contributed to subjects’ recruitment, methodology; Trias Mahmudiono, Ho-Chi Hsu contributed to review, sampling and formal analysis, Wan-Ru Wang, Zhen-Yi Li contributed to data curation, visualization; Hsiu-Ling Chen contributed to conceptualization, methodology, validation, writing – original draft, editing and funding acquisition.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval The study protocol was approved by the Ethics Committee of NCKUS (Tainan, Taiwan, encoded: A-ER-108–189) and TWB (Taipei, Taiwan, encoded: TWBR10811-05) in accordance with the Ethical Principles for Medical Research Involving Human Subjects.
Consent to Participate
All study participants provided written informed consent.
Consent for Publication
No need.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sung, JM., Chang, WH., Liu, KH. et al. The Effect of Co-Exposure to Glyphosate, Cadmium, and Arsenic on Chronic Kidney Disease. Expo Health 14, 779–789 (2022). https://doi.org/10.1007/s12403-021-00451-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12403-021-00451-3